Bone Marrow Transplant: Procedure

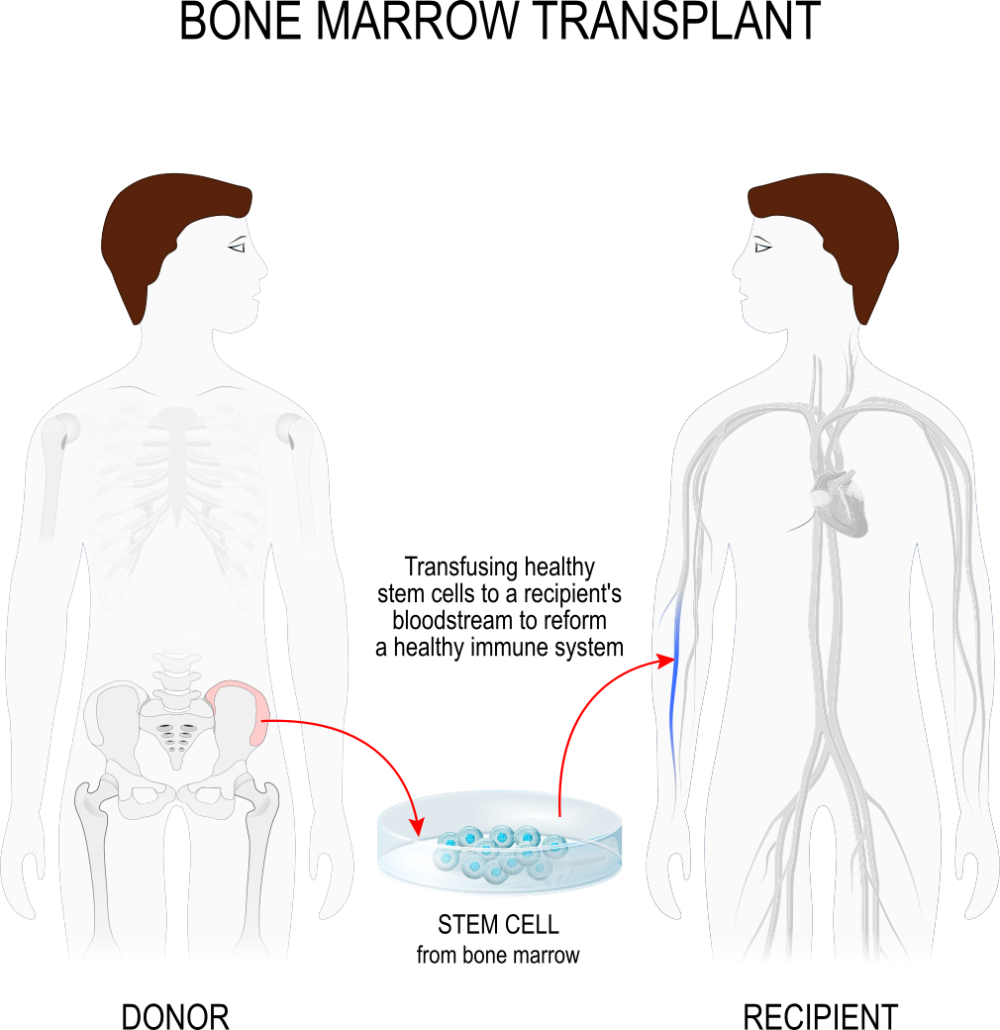
A bone marrow transplant is a treatment that infuses your body with healthy blood-forming stem cells to replace damaged or diseased bone marrow. A stem cell transplant is another name for a bone marrow transplant.
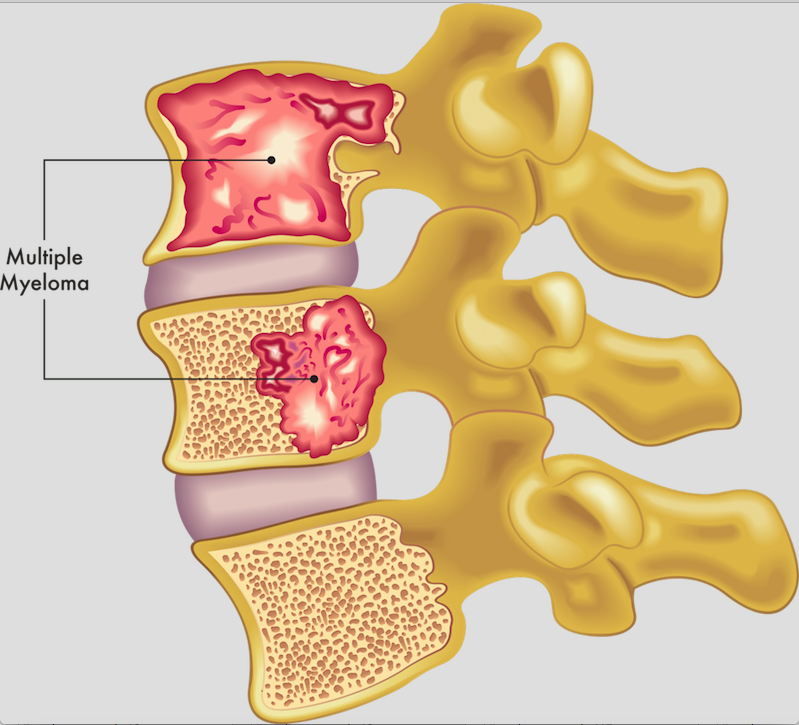
If your bone marrow stops functioning and does not create enough healthy blood cells, you may require a bone marrow transplant.
Bone marrow transplants (allogeneic transplant) use cells from your own body (autologous transplant) or from a donor.
There are three kinds of bone marrow transplants:
Autologous bone marrow transplant:
Also known as Transplantation of autologous bone marrow. The phrase auto refers to oneself. The stem cells destroyed before you take the high-dose chemotherapy or radiation treatment. They then store it in the freezer. The stem cells return to your body after high-dose chemotherapy or radiation treatments to produce normal blood cells. This is a rescue transplant.
Allogeneic bone marrow transplant:
The term allo refers to something different. The extraction of the stem cell from a donor takes places here. In most cases, the donor’s DNA must at least partially match yours. They perform special tests to determine whether a donor is a suitable match for you. A brother or sister is the most likely match. Parents, children, and other relatives are sometimes good matches. National bone marrow registries can help you find donors who are not related to you yet nonetheless match.
Umbilical cord blood transplant:
This is an example of allogeneic transplantation. Right after birth, the extraction of stem cells takes place from a newborn baby’s umbilical cord. The stem cells are frozen and kept in a freezer until they are needed for a transplant. Because umbilical cord blood cells are young, precise matching is not required. Blood counts take substantially longer to recover due to the lower quantity of stem cells.
Preparation for a bone marrow transplant varies based on the kind of transplant, the condition that requires the transplant, and your tolerance for particular medications.
Take into account the following:
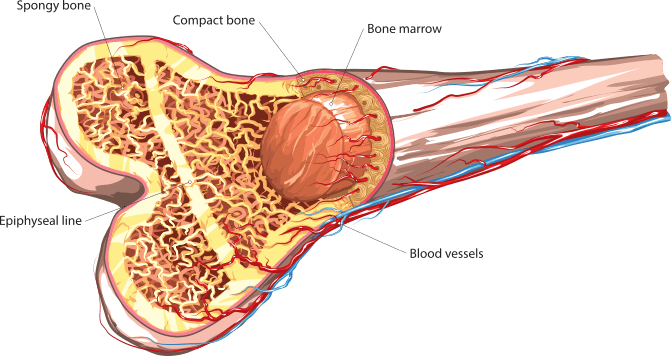
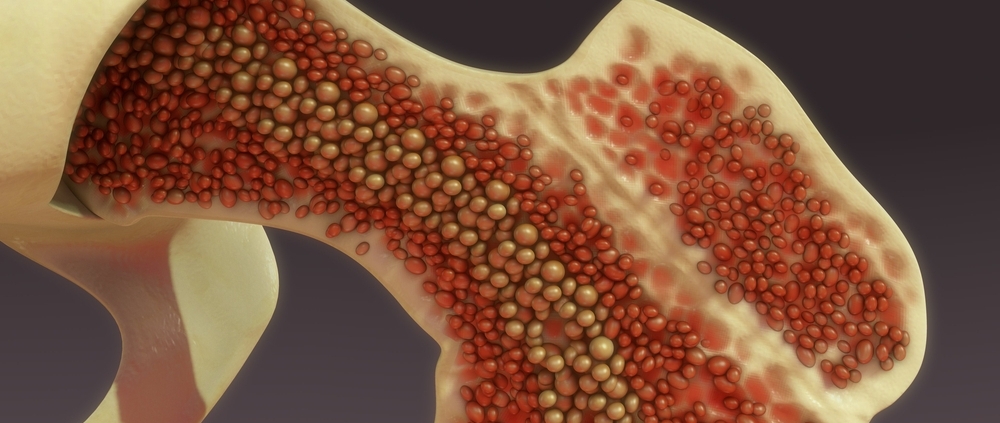
High dosages of chemotherapy and/or radiation are frequently incorporated in the preparations. This aggressive treatment is essential to adequately cure the cancer and provide place in the bone marrow for new cells to proliferate. Because of the impact on the bone marrow, this therapy is sometimes called to as ablative or myeloablative. The bone marrow is responsible for the production of the majority of the blood cells in our bodies. Ablative treatment halts cell creation, and the marrow becomes depleted. To allow the new stem cells to proliferate and form a new blood cell, the marrow must be empty.
Following the administration of chemotherapy and/or radiation, the marrow transplant is infused into the circulation via central venous catheter. Placing the marrow into the bone is not a surgical operation, but rather analogous to having a blood transfusion. The stem cells enter the bone marrow and begin to reproduce and form new, healthy blood cells.
Following the transplant:
Supportive care is provided to prevent and cure infections, treatment side effects, and problems. This involves doing periodic blood tests, closely monitoring vital signs, measuring fluid input and output, weighing patients on a daily basis, and providing a safe and clean environment.
The days leading up to the transplant are considered as negative days. The day of the transplant is regarded as day zero. Plus days are noted for engraftment and recuperation after the transplant. For instance, a patient may be admitted to the hospital on day -8 for a preparatory regimen. The day of the transplant is zero. Days +1, +2, and so on will be added. Each day before, during, and after transplant has its own set of events, difficulties, and hazards. The days are counted to assist the patient and family in understanding where they stand in terms of risks and discharge preparation.
The following symptoms may occur:
- Pain
- Chills
- Fever
- Hives
- Chest pain
- After infusion, the patient may:
- Spend several weeks in the hospital
- Be very susceptible to infection
- Experience excessive bleeding
- Need blood transfusions
- Be confined to a clean environment
- Take multiple antibiotics and other medicines
- If the transplant was allogeneic, you will be given medication to avoid graft-versus-host disease. Even if the donor is a relative, the transplanted new cells (the graft) tend to assault the patient’s tissues (the host).
- Submit to ongoing laboratory testing
- Nausea, vomiting, diarrhoea, mouth sores, and acute weakness are common symptoms.
- Feel brief mental bewilderment as well as emotional or psychological anguish

Following discharge from the hospital, the patient’s recuperation process might last several months or more, during which time the patient cannot return to employment or many formerly loved activities. The patient must also return to the hospital or healthcare provider’s office on a regular basis.














Leave a Reply
Want to join the discussion?Feel free to contribute!