The Fontan Procedure
The severe congenital cardiac problems can now be successfully treated thanks to a surgical approach known as the Fontan procedure. This bears the name of its inventor, Dr. Francis Fontan. Numerous children and adults born with congenital cardiac abnormalities that were formerly thought to be fatal have received lifesaving surgery thanks to it. The Fontan operation will be thoroughly examined in this article. From its historical inception to its contemporary uses, emphasizing its relevance in the field of pediatric cardiology and the care of congenital cardiac disease.
Historical Background
Since its start in the late 1960s, the Fontan technique has advanced significantly. Children born with single-ventricle heart abnormalities had poor prognoses prior to its introduction. Instead of the traditional two functioning ventricles, which make up the heart’s pumping chamber, these anomalies often affect just one. These patients frequently experienced poor oxygenation, restricted exercise tolerance, and a worse quality of life without the Fontan operation.
Overview of the Fontan Process
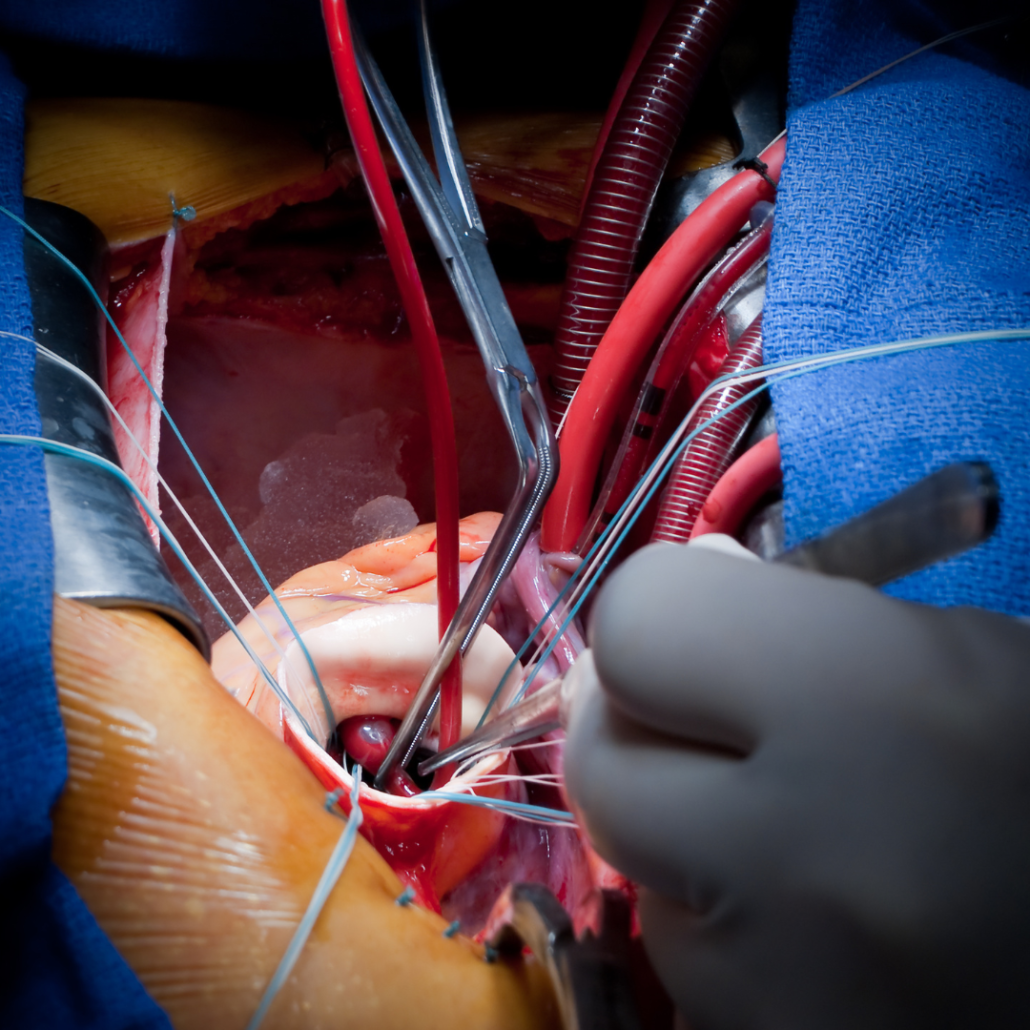
This technique is a phased surgical method that avoids the heart’s damaged ventricle. This is by rerouting venous blood flow to the pulmonary arteries. As a result, the body receives oxygenated blood directly from the lungs, bypassing the undeveloped or malfunctioning ventricle. The following are the main steps in this procedure:
- Stage I: Glenn Shunt or Norwood Procedure:
The superior vena cava (SVC) is surgically connected to the pulmonary artery in the first stage. This normally happens very soon after birth and results in a partial diversion of oxygen-rich blood to the lungs. The Glenn shunt or the Norwood operation are two ways to do this treatment.
- Stage II: Hemi-Fontan or Bidirectional Glenn
Around 4 to 6 months of age is when the second step then takes place on the youngster. It takes place by totally rerouting the SVC to the pulmonary artery in this stage. Thus, more oxygen-rich blood may travel directly to the lungs.
- Stage III: Completion Fontan
This last procedure often takes place when the kid is between the ages of 2 and 4. Here, the pulmonary artery and inferior vena cava (IVC) join together. This allows all deoxygenated blood to bypass the heart and travel straight to the lungs for oxygenation.
Advantages and Drawbacks
Many congenital cardiac patients now have far better quality of life because to the Fontan treatment. They may live and flourish despite having complicated heart architecture thanks to it. The following are some of the main advantages of the procedure:
- Improved Oxygenation: In individuals with single-ventricle heart abnormalities, the surgery improves oxygenation and lessens cyanosis (bluish staining).
- Improved Exercise Tolerance: Children who get the Fontan operation have improved exercise tolerance, which improves their quality of life.
- Prolonged Survival: Many patients with congenital cardiac abnormalities have had their life expectancy extended by the Fontan treatment, enabling them to live into maturity and beyond.
However, the procedure is not without its challenges.
Some of the common issues associated with the fontan surgery include:
- Fontan-Associated Liver Disease (a): The changed blood flow in Fontan patients over time might result in liver issues, needing continued monitoring and possibly therapies.
- Exercise Restrictions: Despite improvements in exercise capacity following the Fontan treatment, patients may still have restrictions during physically demanding activities.
- Long-Term Follow-Up: To treat any problems and make sure the Fontan circulation stays functional, patients need to undergo monitoring by cardiologists and other experts for the rest of their lives.

Modernization of Fontan Surgery
The results of these surgeries have significantly improved thanks to improvements in medical technology and surgical methods. These consist of:
- Minimally Invasive Techniques: Some Fontan treatments may now take place without with the help of minimally invasive methods, obviating the necessity for open heart surgery and speeding up recovery.
- 3D Printing: With the use of 3D printing technology, surgeons may now make patient-specific heart models that can be very helpful for accurate preoperative planning and decreased surgical risks.
- Pharmaceutical Interventions: Ongoing research tries to create drugs and treatments to deal with the long-term consequences linked to the Fontan circulation, including as liver disease and arrhythmias.
The Fontan procedure has been a game-changer in the field of congenital heart surgery. It has offered hope and improved the quality of life for countless individuals born with single-ventricle heart defects. While challenges and long-term complications remain, ongoing research and advancements in surgical techniques continue to push the boundaries of what is possible for patients with this condition. As we look to the future, it is clear that the Fontan procedure will remain a vital lifeline for those in need, offering a chance at a healthier and more fulfilling life.